Does Anthem Health Insurance Cover Covid Testing
According to its website Anthem will cover COVID-19 testing with no out-of-pocket costs when a patient has symptoms of COVID-19 has been exposed to someone who has COVID-19 or if the test is. Check your state guidelines and call the coronavirus testing site before you go to learn about testing criteria availability and hours.
Covid 19 Updates Anthem Blue Cross And Blue Shield Healthcare Solutions
Anthems affiliated health plans will waive cost shares for our fully-insured employer individual Medicare and Medicaid plan membersinclusive of copays coinsurance and deductiblesfor COVID-19 test and visits and services during the visit associated with the COVID-19 test including telehealth visits.
Does anthem health insurance cover covid testing. Will Anthem waive member cost shares related to screening andor testing for COVID-19. All Anthem plans cover medically necessary COVID-19 testing and the care visit where the test takes place with no out-of-pocket costs. That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs.
Find a COVID-19 testing location near you by using this tool. The best way to prevent infection is to get a COVID-19 vaccine. Anthem also confirms that prior authorization is not required for diagnostic services related to COVID-19 testing.
If you dont have symptoms and dont think youve been exposed to someone with COVID-19 but you are an essential worker as discussed below your health plan must cover your COVID-19 test. Insurance Must Cover Covid Tests Even For Asymptomatic Patients CMS Says. In addition UC SHIP will also cover the member cost sharing for COVID-19 treatment from March 9.
Anthems affiliated health plans will waive cost shares for our fully-insured employer individual Medicare and Medicaid plan membersinclusive of copays coinsurance and deductiblesfor COVID-19 test and visits and services during the visit associated with the COVID-19 test. Can I go to a temporary or pop-up COVID-19 testing site. This is because COVID-19 antibodies will start to form whether or not the person has recovered.
All Anthem plans will cover medically necessary screening and testing for COVID-19 and will waive all cost shares co-pays coinsurance and deductibles. A doctor must order a COVID-19 test. But Washington states COVID-19 testing requirements which have been extended through July 3 do apply to short-term health plans requiring them to cover testing with no cost-sharing just like other health plans North Dakotas bulletin also applies to short-term plans but it asks rather than requires insurers to waive cost-sharing for COVID-19 testing.
Many Anthem health clinics doctors offices and the health department offer HIV testing. COVID-19 Test Site Finder. You will need an appointment for most of these sites.
COVID-19 testing and visits associated with COVID-19 testing. COVID-19 testing at temporary or pop-up testing sites is covered by Blue Shield and Blue Shield Promise without out-of-pocket costs. Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a.
You may also have to fill out a. Waiving cost-sharing for COVID-19 testing and treatment. However you must contact your.
COVID-19 under federal law you can obtain a COVID -19 test anywhere and your health plan must pay for the test. Waiving all prior authorization requirements for COVID-19 testing and related covered services. Following a national trend two of Maines largest health insurance providers Anthem and Harvard Pilgrim have stopped waiving patients out-of-pocket costs such as deductibles and copayments for COVID-19-related treatment meaning that patients hospitalized for the illness will likely have to pay a lot more.
Health insurance companies declared they would cover 100 of the costs for COVID treatment waiving copays and. Am I covered for a COVID-19 test or screening. Anthem building in Indianapolis.
Some pharmacies with on-site clinics may also be able to give HIV testing. Even though some clinics accept walk-in appointments making an appointment ahead of time will save you time and ensure that you receive your test on the same day. Indianapolis based Anthem Insurance announced Friday the company will begin providing coverage of the coronavirus screening test at no out-of-pocket-cost.
Coronavirus test criteria and availability are changing daily. If youre traveling youll want to visit. Yes as of March 5 2020 and until further notice cost shares including copays coinsurance and deductibles for COVID-19 will be waived by Anthem or its delegated entities for screening and testing for COVID-19.
Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021. This includes screenings andor tests that take place at in-person office visits drive-through sites virtual on-line visits and telephone calls. Some health insurers ending waivers for Covid treatment fees Waivers have meant substantial savings for Covid-19 patients who fall seriously ill and wind up in the hospital.
There should be no additional cost sharing for diagnostic covid-19 testing. Anthem insurance plans providing COVID-19 testing at no charge. Check the CDC website for up-to-date information.
The FDA has authorized three vaccines that have proven to be up to 95 effective in protecting against COVID-19. UC SHIP will eliminate member cost sharing to 0 for all medically necessary screening and testing for COVID-19 until further notice. In 2020 as the pandemic took hold US.
The company recommends using telehealth when possible to help prevent the spread of a virus. Please talk to a doctor first to be certain you need a COVID-19 test. According to the CDC antibody testing may help support a diagnosis of COVID-19 in people who continue to experience symptoms many days or weeks after the symptoms started.
Anthem will cover the cost of coronavirus testing with no out-of-pocket cost.
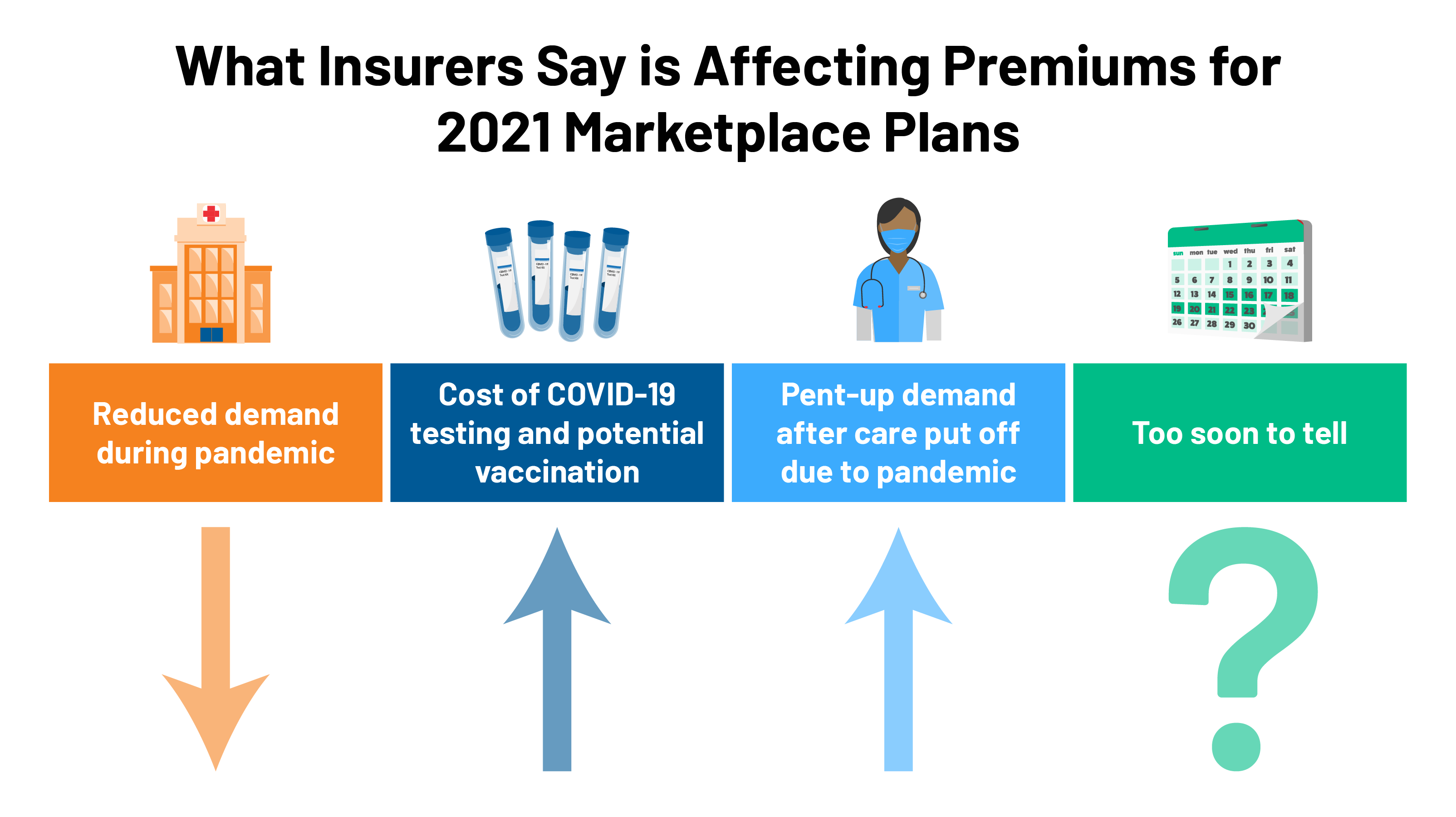
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff
Anthem Says Covid 19 Costs Could Rise In Coming Quarters From Variants Reuters
Coronavirus Covid 19 Information For Individual Family And Employer Group Plans Anthem Blue Cross
Coronavirus Covid 19 Information For Employers Producers Anthem Blue Cross
Anthem Blue Cross Plans Will Waive Out Of Pocket Costs For Coronavirus Treatment
Well Being Incentives Be Well Shbp
Anthem Insurance Coverage For Drug And Alcohol Rehab Treatment
Small Group Health Insurance With Chamberadvantage Kentucky Chamber
Informacion Sobre El Coronavirus Covid 19 Para Planes Individuales Y Familiares Y Planes Grupales De Empleadores Anthem Blue Cross
Anthem Blue Cross Introduces New Narrow Network For 2021
Anthem Says Covid 19 Costs Could Rise In Coming Quarters From Variants Reuters
Anthem Connecticare Seek Premium Increases For 2021 Health Plans Anthem Connecticare Seek Premium Increases On Ct Public Exchange Health Plans
Anthem Blue Cross Woodland Hills Ca Warner Plaza Urgent Care
Anthem Blue Cross Healthcare Insurance Xpress Urgent Care
Anthem Blue Cross And Blue Shield Foundation Vivent Health
Insurance Companies Are Requesting Higher Rates For Health Plans Next Year
Covid 19 Testing Requirements Anthem Com Ca



Posting Komentar untuk "Does Anthem Health Insurance Cover Covid Testing"