Does Cigna Health Insurance Cover Covid Testing
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. Cigna Expands and Extends COVID-19 Relief Efforts for Medicare Advantage and Individual and Family Plans.
Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
Does Cigna Cover Covid testing at urgent care.
Does cigna health insurance cover covid testing. You have options Cigna is waiving out-of-pocket costs for COVID-19 visits whether. The company will reimburse health care providers at Cignas in-network rates or Medicare rates as applicable. In Vitro Diagnostic Testing coverage policy for additional coverage criteria.
Most plans however will not cover a COVID-19 test if you are asymptomatic or if you just feel like it. Section 6001 of the Families First Act as amended by the CARES Act requires private health insurance plans to cover testing needed to detect. Cigna Covers Cost Of Coronavirus Tests For Customers.
Thats because federal law requires insurers to waive costs for covid testing and vaccination. Cigna is waiving out-of-pocket costs for office visits related to testing and diagnostic tests for COVID-19 as required by the CARES Act. Self-insured group health plans administered.
There are 2 types of COVID-19 tests. A complaint was filed today against Cigna Health and Life Insurance by Murphy Medical Associates regarding the provision of COVID-19 testing in the state of Connecticut. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021.
November 6 2020. You will be responsible for any testing costs related to non-diagnostic COVID-19 tests and the cost of the visit associated with the test will be covered according to your plans normal cost-share. Many insurers youve seen in the news like Blue Cross Blue Shield Aetna and Cigna have announced that if you or someone in your.
Oscar does not cover COVID-19 antibody tests if they are administered outside of these settings because they are not used to diagnose COVID-19 or determine a course of treatment. Last updated August 23 2021 Highlighted text indicates updates On July 19 2021 the Secretary of Health and Human Services HHS renewed the national public health emergency PHE period for COVID-19 through October 17 2021. New Cigna Care Card to Help Clients Provide Financial Assistance to Employees Impacted By COVID-19.
The treatments that Cigna will cover for COVID-19 are those covered under Medicare or other applicable state regulations. We encourage you and your health care provider to use FDA-authorized tests. In all cases providers should bill the COVID-19 test with the diagnosis code that is appropriate for the reason for the test.
BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. Connect with a provider. Cigna Coronavirus COVID-19 Interim Billing Guidance for Providers for Commercial Customers.
Access testing if you need it Cigna is waiving out-of-pocket costs for FDA-approved COVID-19 diagnostic PCR and antigen testing tests. Cigna Health does not specify. Diagnostic tests determine if you are currently infected with COVID-19.
Enhanced coverage for COVID-19 diagnostic testing office exams telehealth screenings and virtual care applies to customers in the United States who are covered under Cignas employerunion sponsored insured group health plans insured plans for globally mobile individuals Medicare Advantage Medicaid and the Individual and Family insurance plans. Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles. Consistent with the new end of the PHE period Cigna.
Please review our COVID-19. Cigna will determine coverage for each test based on the specific codes that the. Insurers must cover the cost of the diagnostic testing even if the person just wants for example to be sure that they dont have COVID before visiting friends or family members insurers are not required to cover the cost of widespread COVID testing thats done for public health surveillance or employment purposes although they can choose to collaborate with public health departments or.
Another common exclusion to getting an insurance company to pay for your coronavirus test is when there is a hospital requirement for a negative COVID-19 test before an unrelated or not covered in your plan medical procedure. Can I go to a temporary or pop-up COVID-19 testing site. Plans and issuers are not required to provide coverage for this type of COVID-19 testing.
You will need an appointment for most of these sites. You may also have to fill out a. Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers whether at a providers office urgent care center emergency room or via virtual care through the Public Health Emergency PHE period currently scheduled to end on October 18 2021.
Cigna Launches Real-Time Digital. Or public health surveillance and antibody tests are not covered by Cignas standard coverage but may be covered as required by state law. COVID-19 testing at temporary or pop-up testing sites is covered by Blue Shield and Blue Shield Promise without out-of-pocket costs.
According to its website Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing through Jan. Testing for COVID-19 is important to slowing the spread of COVID-19. Cigna is facing a lawsuit arguing it failed to pay a New Jersey medical office for COVID-19 diagnostic testing and treatment according to a complaint filed this week in federal court.
Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. CI customers will have access to coronavirus COVID-19 testing as prescribed by health practitioners and the company will waive all co-pays or cost-shares to help fight the rapid spread of the virus in the.
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff
Most People Won T Have To Pay For Covid 19 Testing Coronavirus
Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
Insurance Carecube We Take Most Of Major Insurances
Covid 19 Resources For Health Care Access In Washington State Northwest Health Law Advocates
Cigna Requires Employees Returning To Office To Be Fully Vaccinated Reuters
What To Know About Coronavirus Your Insurance Utah Insurance Department
Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
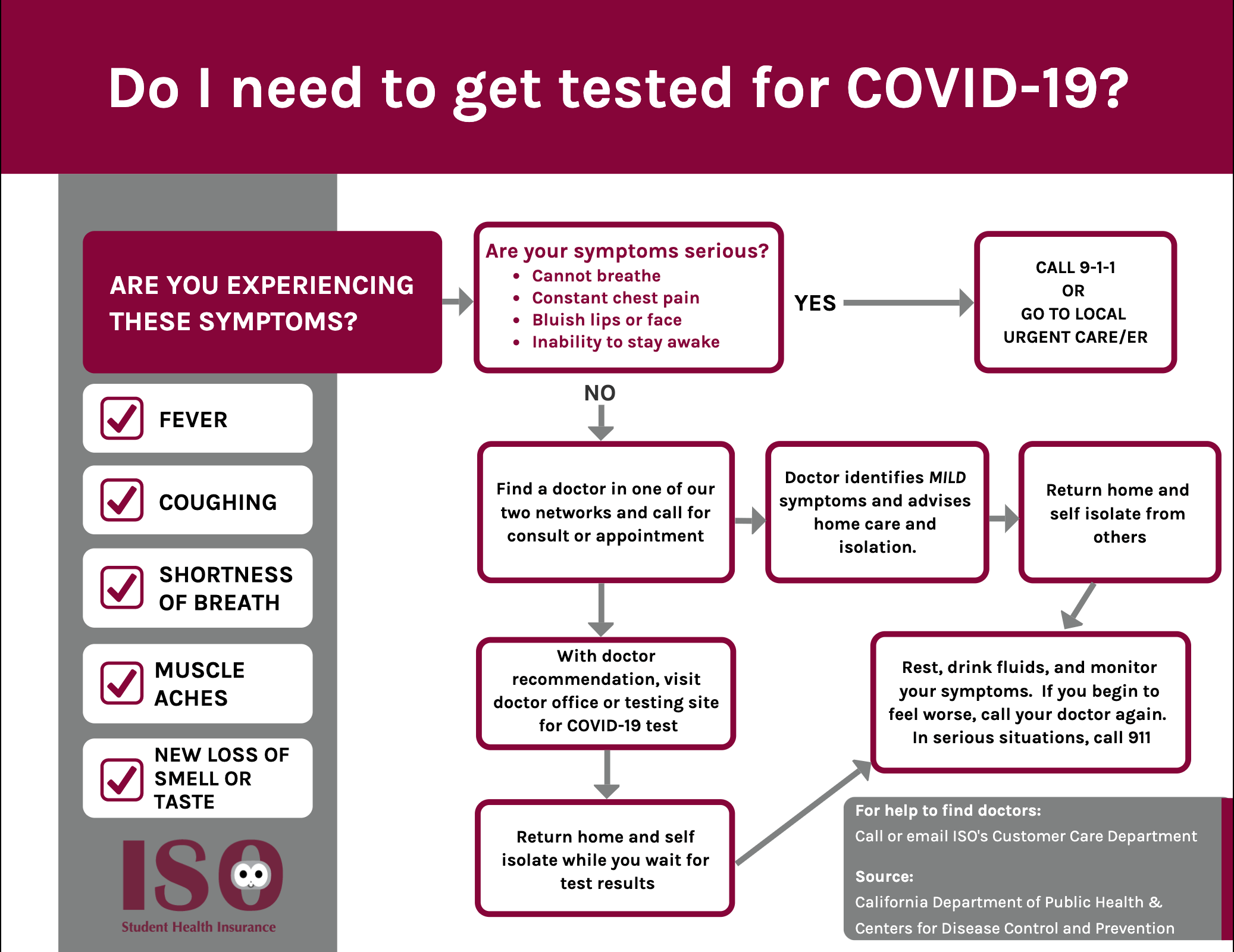
Iso International Student Insurance
Covid 19 Pruebas Tratamiento Y Cobertura De La Vacuna Cigna
Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
Cigna And Humana Waive Coronavirus Treatment Costs
Cigna Protects Its Workforce By Requiring Covid 19 Vaccinations Or Testing For Employees Entering U S Worksites
Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
Manipal Cigna Health Insurance Plans Reviews And Premium Calculator




Posting Komentar untuk "Does Cigna Health Insurance Cover Covid Testing"