Does Aetna Cover Covid Testing
Diagnostic tests determine if you are currently infected with COVID-19. Both labs also offer antibody testing to detect the presence of antibodies to SARS-CoV-2.
UnitedHealthcare is updating testing guidelines coding and reimbursement information for the COVID-19 health emergency based on guidance from the Centers for Medicare Medicaid Services CMS the Centers for Disease Control and Prevention CDC state and federal governments and other health agencies.
Does aetna cover covid testing. Medicaid members do not have copays for these services. And second youre in luck. 1-800-557-6059 TTY 711 247.
Most plans however will not cover a COVID-19 test if you are asymptomatic or if you just feel like it. Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings. This policy covers the cost of the office clinic or emergency room visit that results in the administration of or order for a COVID-19 test.
Some countries require COVID-19 testing for travelers on arrival. If you have Aetna health insurance you can visit their site here to review Testing Treatment FAQs which include details about coverage and authorizations for COVID-19 expenses. And its subsidiary companies are not responsible or liable for the content accuracy or privacy practices of linked.
To ensure access for COVID-19 testing and have consistent reimbursement Aetna will reimburse contracted and non-contracted providers for COVID-19 testing as follows in accordance with the members benefit plan 3. Learn about extra benefits and well-being resources just for you find testing locations get answers to the most frequently asked questions regarding COVID-19 and tips to stay safe and much more. You are now being directed to the CVS Health COVID-19 testing site Links to various non-Aetna sites are provided for your convenience only.
Aetna is not limiting the number of diagnostic testing we will cover for members however all tests must still meet the requirements listed in this section for coverage. The presence of antibodies can identify who may have recovered from a recent or prior infection and may possibly. Aetna Better Health and Aetna Better Health Kids covers testing screening and office visits to diagnose or treat COVID-19.
You will be responsible for any testing costs related to non-diagnostic COVID-19 tests and the cost of the visit associated with the test will be covered according to your plans normal cost-share. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021. Aetna will waive co-pays for all SARS-CoV-2 testing for all insured enrollees whether the enrollees are in commercial Medicare or Medicaid plans.
And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19. Oscar does not cover COVID-19 antibody tests if they are administered outside of these settings because they are not used to diagnose COVID-19 or determine a course of treatment. Medicare Part B Medical Insurance Part B covers certain doctors services outpatient care medical supplies and preventive services.
Aetna does not require a physicians referral to cover Covid-19 testing. Aetna will waive member cost sharing for diagnostic testing related to COVID-19. In addition Aetna is waiving member cost-sharing for diagnostic testing related to COVID-19.
Self-insured employers can opt-in. We suggest you check directly with them to learn more about your coverage. Empire Blue Cross Blue Shield which covers 4 million New Yorkers does said spokeswoman Alessandra Simkin.
Aetna does not require a physicians referral to cover Covid-19 testing. Will mandatory testing be covered. Will members have co -pays for COVID -19 related services.
CHIP members are not to be charged their standard copayments for testing screening or office visits related to COVID-19. Most health insurance providers have waived costs related to the testing and treatment of COVID-19. First youre doing the smart thing by getting tested before traveling.
Covers a COVID-19 antibody or serology test. According to its website as of Nov. The test can be done by any authorized testing facility.
Labs offer COVID-19 test options. Most Payers Cover Member Costs for COVID-19 Testing Treatment Members may access the at-home test kits or the drive-thru testing option by first completing the. What should I do if my insurance wont cover COVID-19 testing or treatment.
Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you. The test can be done by any approved laboratory. There are 2 types of COVID-19 tests.
Will antibody testing be covered. Testing for COVID-19 is important to slowing the spread of COVID-19. The following rates are used for COVID-19 testing for commercial and Medicare plans unless noted otherwise.
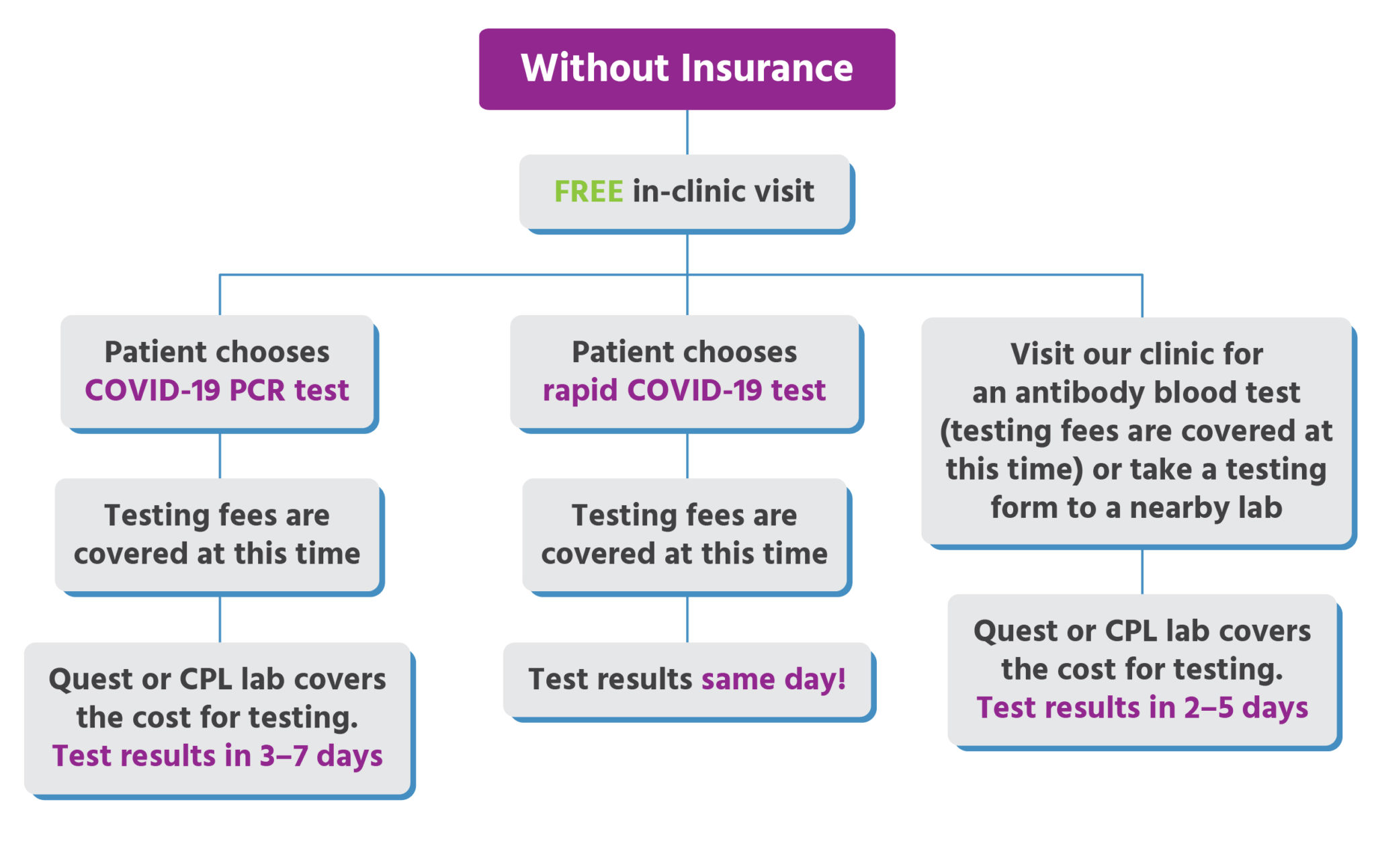
As stated above we only cover COVID-19 diagnostic testing when a member has been referred by a licensed physician. If you have an excepted benefit policy short-term limited duration health insurance coverage or a health care sharing ministry plan you are considered uninsured and the Families First Coronavirus Response Act may provide options to cover your COVID-19 testing. Both Quest Diagnostics and LabCorp offer molecular COVID-19 testing to detect a current SARS-CoV-2 infection.
Aetna is here for you during the coronavirus COVID-19 pandemic no matter what. Empire Blue Cross Blue Shield which covers 4 million New Yorkers does said spokeswoman Alessandra Simkin. Coronavirus disease 2019 COVID-19 antibody test.
Testing to determine if a member has had COVID-19 previously and has developed antibodies against it even on the advice of a medical practitioner. We dont cover COVID-19 antibody testing ie. 9 2020 Aetna is waiving member cost-sharing for diagnostic testing related to COVID-19 done by any.
We encourage you and your health care provider to use FDA-authorized tests. Check back often for updates. This member cost-sharing waiver applies to all Commercial Medicare and Medicaid lines of business.
High risk is defined as aged 65 years or over. Their responses to COVID-19 can be found below and will be updated when new information is provided by insurers. Another common exclusion to getting an insurance company to pay for your coronavirus test is when there is a hospital requirement for a negative COVID-19 test before an unrelated or not covered in your plan medical procedure.

Telehealth And Covid 19 Billing And Coding Resources
Coronavirus Resources Anaheim Ca Official Website

Aetna Para Proveedores Del Cuidado De Salud Recursos Y Apoyo Para Profesionales De La Salud
Urgent Care For Kids Insurance Accepted Cost
Health Care Plan Benefits Human Resources Vanderbilt University
Your Pregnancy Journey Understanding Major Milestones Aetna

Aetna Cigna And Humana Waive Most Costs To Patients For Covid 19 Treatment Shots Health News Npr
Aetna Waives Co Pays For Covid 19 Screenings News Vanderbilt University

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

Covid 19 Testing Bills Surprise New Yorkers Crain S New York Business

Cvs Health Announces Availability Of Covid 19 Antibody Testing At Minuteclinic Locations Across The Country Cvs Health
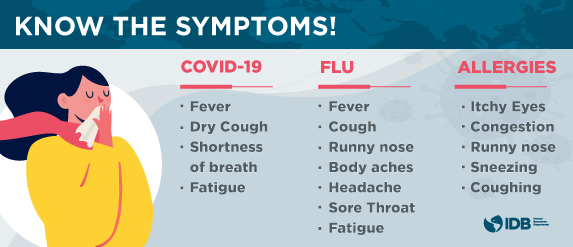
Covid 19 Coronavirus Information Page Iadb

Covid Testing Care Station Medical Group

Planes De Seguro De Salud Individuales Y Familiares Aetna

Posting Komentar untuk "Does Aetna Cover Covid Testing"