Does Cigna Cover Covid Testing
Diagnostic testing for COVID-19 molecular or antigen diagnostic tests including rapid tests saliva tests etc is covered without cost-share prior authorization or other medical management requirements through October 17 2021. The COVID-19 global pandemic is impacting people from all walks of life and people might worry about losing their job or income if they are diagnosed with COVID-19.

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
You will be responsible for any testing costs related to non-diagnostic COVID-19 tests and the cost of the visit associated with the test will be covered according to your plans normal cost-share.
Does cigna cover covid testing. HR6201 does not apply to short-term health plans healthcare sharing ministry plans or other health plans that arent considered minimum essential coverage. New Cigna Care Card to Help Clients Provide Financial Assistance to Employees Impacted By COVID-19. If as part of that visit the provider administers or orders a test for influenza strep or other respiratory infection that additional testing will also be covered without member cost sharing.
COVID-19 testing sites near me in your internet browser. Or public health surveillance and antibody tests are not covered by Cignas standard coverage but may be covered as required by state law. Self-initiated at-home specimen collection kits that are FDA-approved such as the Pixel by LabCorp testing kit will be covered by Cigna cost share waived.
Humana Medicare Advantage and Medicaid members. Together were preventing diagnosing and treating diseases with greater precision an approach we call The Keck Effect. Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a.
There are 2 types of COVID-19 tests. CI customers will have access to coronavirus COVID-19 testing as prescribed. March 5 2020 PRNewswire -- Cigna NYSE.
Consistent with the new end of the PHE period Cigna is extending cost-share waivers for COVID-19 diagnostic testing and related office visits through October 17 2021. BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. We cover without member cost sharing a same day office emergency room or other provider visit at which a COVID-19 test is ordered or administered.
We encourage you and your health care provider to use FDA-authorized tests. CI customers will have access to coronavirus COVID-19 testing as prescribed by health practitioners and the company will waive all co-pays or cost-shares to help fight the rapid spread of the virus in the US. About Keck Medicine of USC The Keck Effect Keck Medicine of USC is a world-class academic medical center that attracts the worlds top physicians and researchers.
Results are available in 1-3 days after sample is received at lab. At Cigna we strive to safeguard your health and remain true to our mission which is to help improve your health well-being and peace of mind. Cigna Expands and Extends COVID-19 Relief Efforts for Medicare Advantage and Individual and Family Plans.
November 6 2020. Cigna is facing a lawsuit arguing it failed to pay a New Jersey medical office for COVID-19 diagnostic testing and treatment according to a complaint filed this week in federal court. According to its website Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing through Jan.
05132020 2020 Cigna. The federal government had to step in to require self-insured plans to fully cover COVID-19 testing and to address the issue in the states that hadnt taken action on their own. Cigna Launches Real-Time Digital.
Will Humana cover Covid-19 testing. Our world-class medical facilities are staffed by over 500 physicians. Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles.
Diagnostic tests determine if you are currently infected with COVID-19. Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. We also continue to make additional key accommodations as outlined on this page.
Cigna Health does not specify a limit on the number of COVID-19 tests it. Humana Commercial Group members. Under the terms of the Families First Coronavirus Response Act HR6201 Medicare Medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of COVID-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most recently been extended through mid-April 2021.
Oscar does not cover COVID-19 antibody tests if they are administered outside of these settings because they are not used to diagnose COVID-19 or determine a course of treatment. In COVID-19 admissions Cigna will allow direct emergent or urgent transfers from an acute inpatient facility to a second acute inpatient facility skilled nursing facility SNF acute rehabilitation. A complaint was filed today against Cigna Health and Life Insurance by Murphy Medical Associates regarding the provision of COVID-19 testing in the state of Connecticut.
Effective today Cigna is waiving customer cost-sharing for all COVID-19 treatment through May 31 2020. Cigna Covers Cost Of Coronavirus Tests For Customers Business Financial BLOOMFIELD Conn. During the public health emergency there will be no out-of-pocket costs for Humana Medicare Advantage and Medicaid members who receive a US Food Drug Administration FDA approved or emergency use authorized COVID-19 test opens new window.
CIGNA SPECIAL COVERAGE FOR COVID19-Client-Level Snapshot. Cigna Waives Customer Cost-Sharing for COVID-19 Treatment. The treatments that Cigna will cover for COVID-19 are those covered under Medicare or other applicable state regulations.
Testing for COVID-19 is important to slowing the spread of COVID-19. And for its globally mobile customers. Cigna is waiving out-of-pocket costs for office visits related to testing and diagnostic tests for COVID-19 as required by the CARES Act.
How is Cigna covering COVID-19 testing.

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
:format(jpg)/https://f.elconfidencial.com/original/d9a/b51/1ac/d9ab511ac9e60dca299584c16d793e02.jpg)
Quien Tiene Que Pagar Los Test Pcr De Coronavirus Que Las Empresas Hacen A Sus Trabajadores

Cigna Requires Employees Returning To Office To Be Fully Vaccinated Reuters

Cigna And Humana Waive Coronavirus Treatment Costs

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
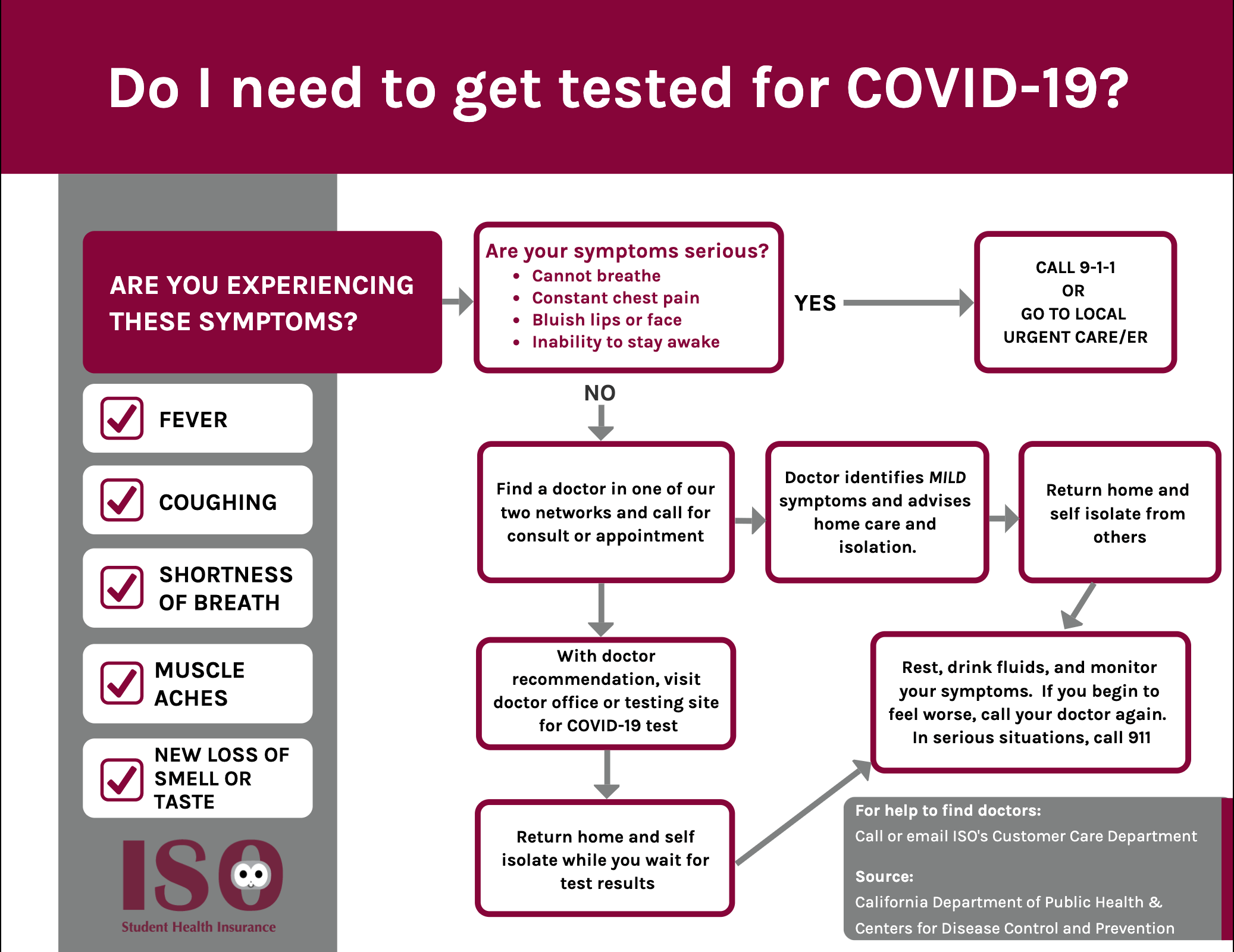
Iso International Student Insurance

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna
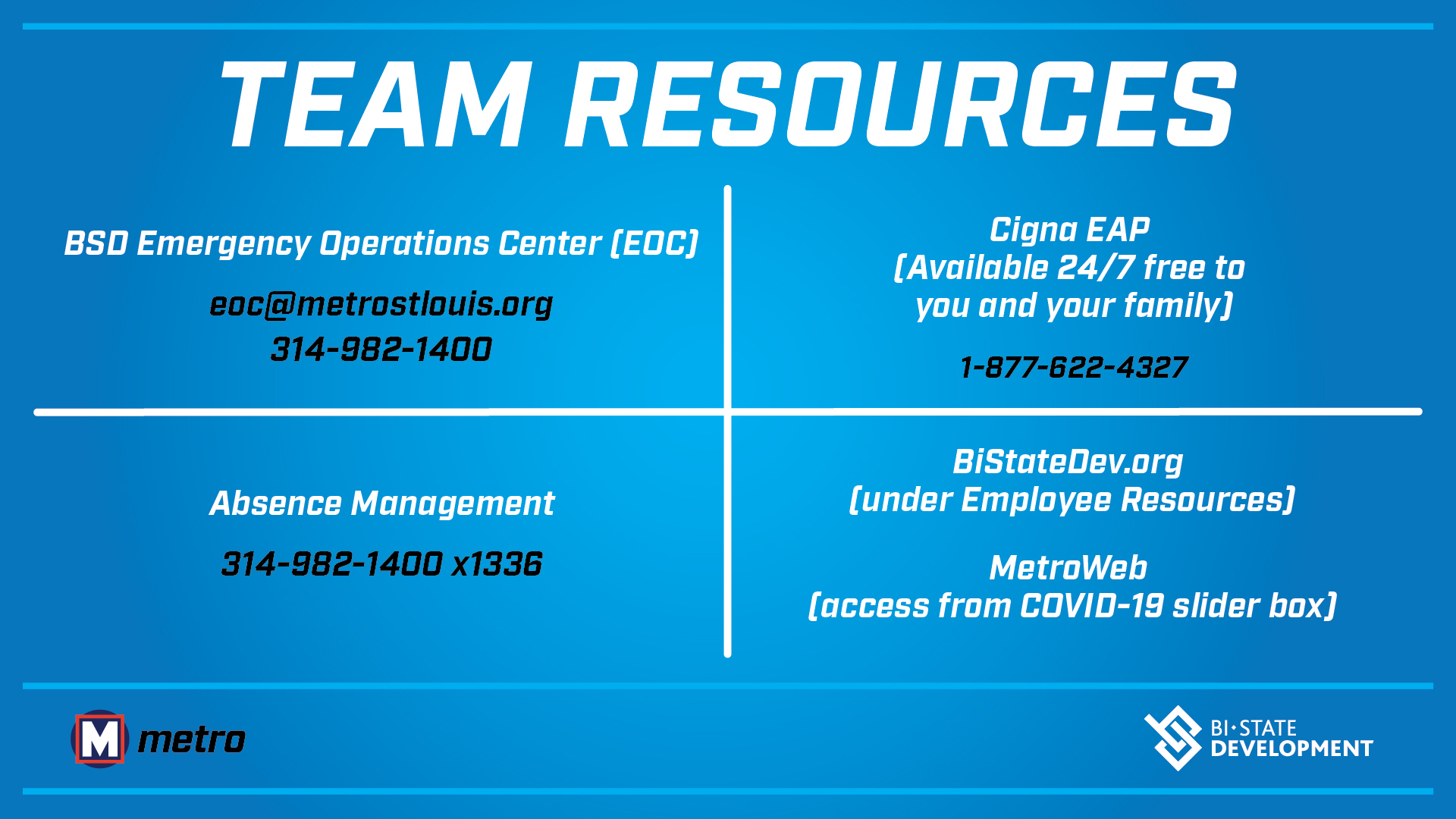
Coronavirus Covid 19 Information Bsd
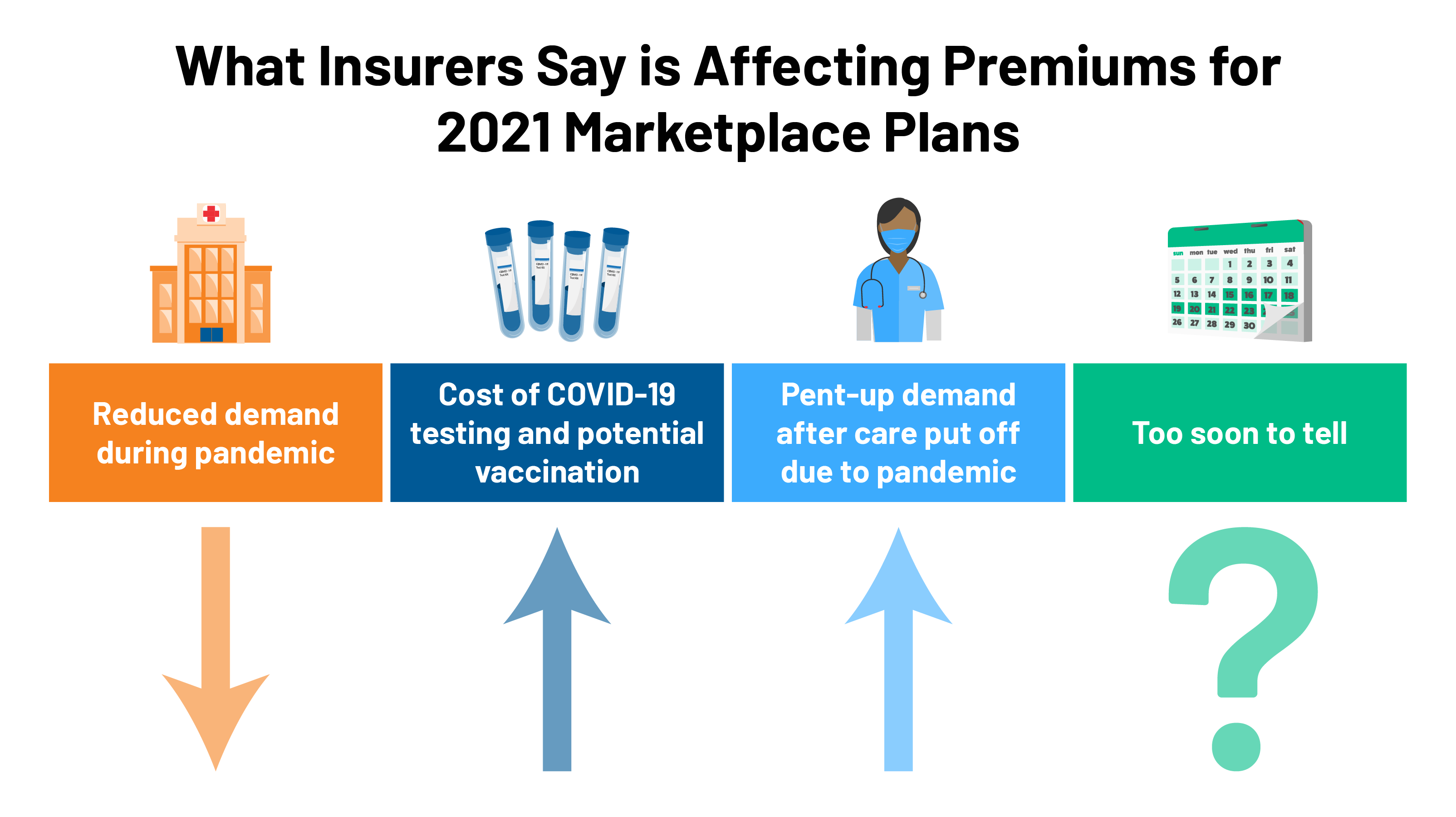
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Covid 19 Pruebas Tratamiento Y Cobertura De La Vacuna Cigna

What To Know About Coronavirus Your Insurance Utah Insurance Department
Posting Komentar untuk "Does Cigna Cover Covid Testing"