Does Blue Cross Complete Cover Covid Testing
Yes COVID-19 test fees are considered eligible to deduct as a medical expense by the Canadian Revenue Agency under a Health Spending Account when accompanied with a prescription from a medical doctor pharmacist nurse or dentist. Any costs related to delays caused by testing requirements.
All Anthem plans cover medically necessary COVID-19 testing and the care visit where the test takes place with no out-of-pocket costs.

Does blue cross complete cover covid testing. Lab tests are only considered when they are ordered by a doctor in an acute medical emergency situation. Any COVID-19 testing including those required by governments to re-enter the country. You must be a Blue Cross and Blue Shield Service Benefit Plan member 18 or older with a MyBlue account to earn this reward.
For commercial members when an attending health care provider administers or refers a patient for COVID-19 testing Blue Cross and BCN assume the health care provider has determined the test to be. We suggest you bill Blue Cross or BCN first for COVID -19-related services and wait for the voucher remittance advice to determine member cost share liability. Lab tests to diagnose COVID-19 are covered at no cost.
Please talk to a doctor first to be certain you need a COVID-19 test. Blue Cross and Blue Shield Companies Announce Coverage of Coronavirus Testing for Members and Other Steps to Expand Access to Coronavirus Care CHICAGO -- Blue Cross Blue Shield Association BCBSA announced today that its network of 36 independent and locally-operated Blue Cross and Blue Shield BCBS companies will waive prior authorizations and increase coverage for COVID-19 as. Does Blue Shield and.
Eligible members will earn the incentive when they provide proof of getting at least one COVID-19 vaccine dose by December 31. Premera Blue Cross is here to support members employers and healthcare providers during the coronavirus COVID-19 outbreak. BCBSTX is waiving your share of the costs for COVID-19 testing and testing-related visits until the end of the Health and Human Services COVID-19 public health emergency order.
It is possible that having been infected by COVID-19 will reduce your chance of being infected in the future but researchers do not yet have a reliable way of knowing who is protected or for how long Otenti said. COVID-19 testing is available at no cost. COVID-19 Blue Cross and Blue Shield of Texas This page may have documents that cant be read by screen reader software.
Updated Mar 6 2020 209pm EST. Does Alberta Blue Cross cover COVID-19 testing when I am at the destination. Any costs related to quarantines including those mandated by governments.
Medavie Blue Cross travel insurance does not cover. More than 140 million Americans have received a dose of the COVID-19 vaccine. For testing performed out of network CareFirst or the plan sponsor will pay 100 up to charge.
Do your part and get vaccinated by December 31 2021. People who recover from COVID-19 have antibodies to the virus that remain in the plasma portion of their blood. Eligible members can earn 50 on their MyBlue Wellness Card when they submit their vaccination record.
For help with these documents please call 1-800-975-6314. CareFirst and plan sponsors will cover the full cost of in-network deductibles copays and coinsurance for FDA-authorized and medically necessary antibody testing when ordered by a doctor nurse practitioner or other authorized provider. This is what many people want to know but the answer is there is currently no clear answer.
If you charge the member a cost share at the time of service you may need to reimburse the member when you receive your voucher. Find a COVID-19 testing location near you by using this tool. The vaccines are our most powerful tool to stop the spread of COVID-19.
Thats a big step toward stopping the spread of the virus. This includes the contract holder spouse and dependents. However we do cover the cost of testing if a health care provider orders an FDA-approved test and determines that the test is medically necessary.
Florida Blue will cover an FDA-approved antibody test if your doctor has seen you and believes theres a medical reason for the test. Help speed access to COVID-19 testing and treatment and encourage the use of telehealth instead of in person visits to stop the spread of COVID-19. And UPMC Health Plan both said Friday they would cover the cost of testing for COVID-19 for its.
No Blue Cross doesnt cover the cost of workplace or occupational screening tests for COVID-19. Updates as of September 30 2021 Prior authorization requirements waived for transfers to home health or SNF facilities through October 31 2021. La Cañada Querétaro LLDM El Marques Queretaro De Arteaga Mexico.
A doctor must order a COVID-19 test for you. Be provided and the cost-share will be waived for any claim that comes in for COVID-19 testing that is provided by or with a referral from a licensed or authorized health care provider through the end of the federal public health emergency. Blood plasma called convalescent plasma collected from these individuals is being used to treat patients who are ill due to COVID-19.
Your Pacific Blue Cross travel or Visitor to Canada plan does not cover the cost of the COVID test. But some are still hesitant to get the shot. Who can get tested for COVID-19.
Blue Cross and BCN continue to cover COVID-19 testing that is considered medically necessary by an attending health care provider. 1441 likes 38 talking about this 22 were here. Therefore Blue Cross plans will cover outpatient COVID-19 testing and treatment as well as all telehealth visits without charging members any.
The incentive is available to all members covered under Standard Option Basic Option or FEP Blue Focus who are 18 and over and who must have a MyBlue account. Does the presence of antibodies mean immunity. A nurse case manager with Blue Cross Blue Shield of Rhode Island found that listening without judgment to one patients concerns made all the difference.
Blue Shield will not cover antibody tests unless ordered by a healthcare provider licensed to order COVID-19 tests and for a rare case in which it is needed to help make a diagnosis. In keeping with CMS guidance issued September 2 2020 and for the duration of the COVID-19 public health emergency Blue Cross will cover without a healthcare professionals order the cost of one diagnostic test for COVID-19 and one diagnostic test each for influenza virus or similar respiratory condition for Medicare members when performed in conjunction with a COVID-19 test and needed to.

Covid 19 Testing In Puerto Vallarta Vallarta Adventures
Covid 19 Testing In Puerto Vallarta Vallarta Adventures
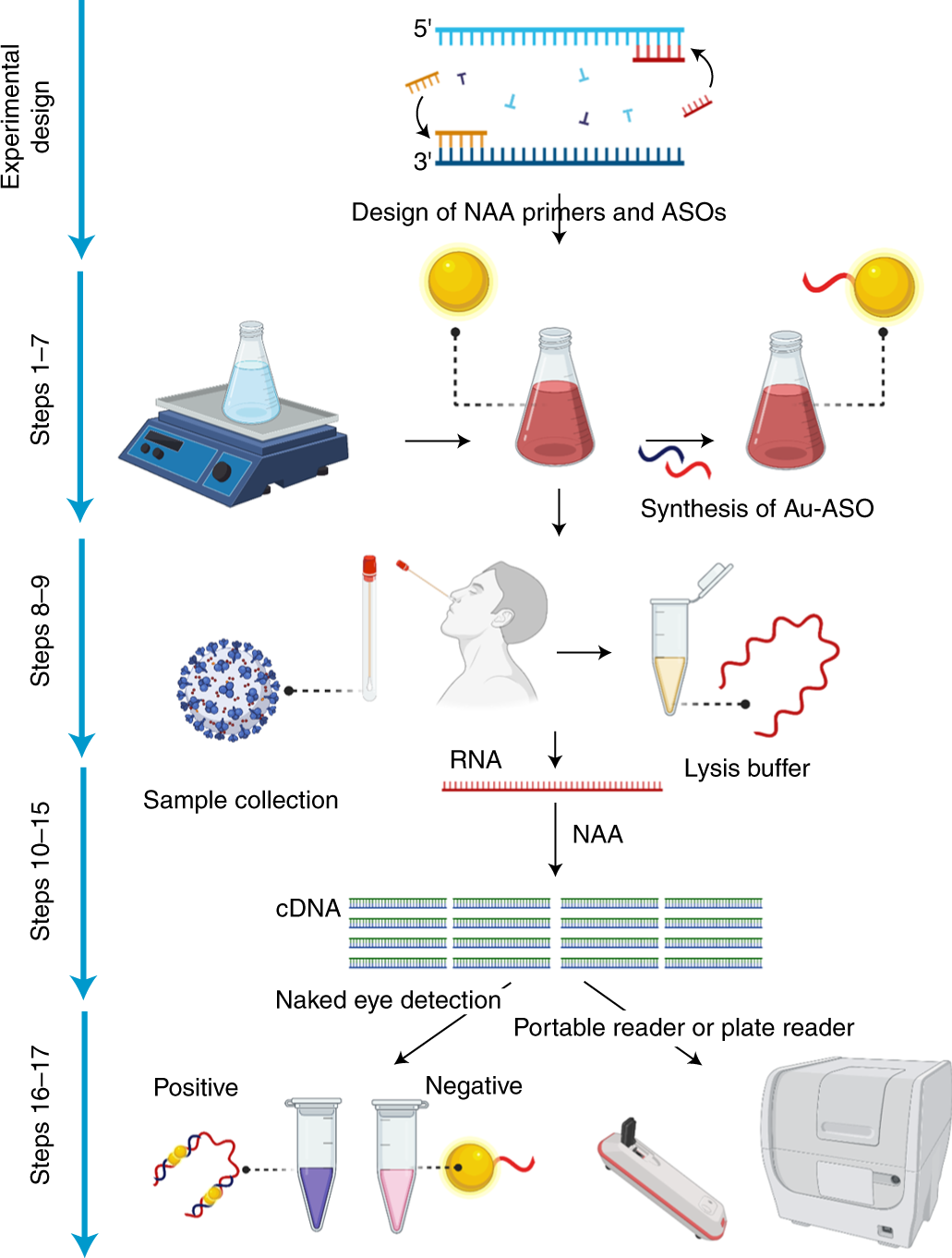
Rna Extraction Free Nano Amplified Colorimetric Test For Point Of Care Clinical Diagnosis Of Covid 19 Nature Protocols
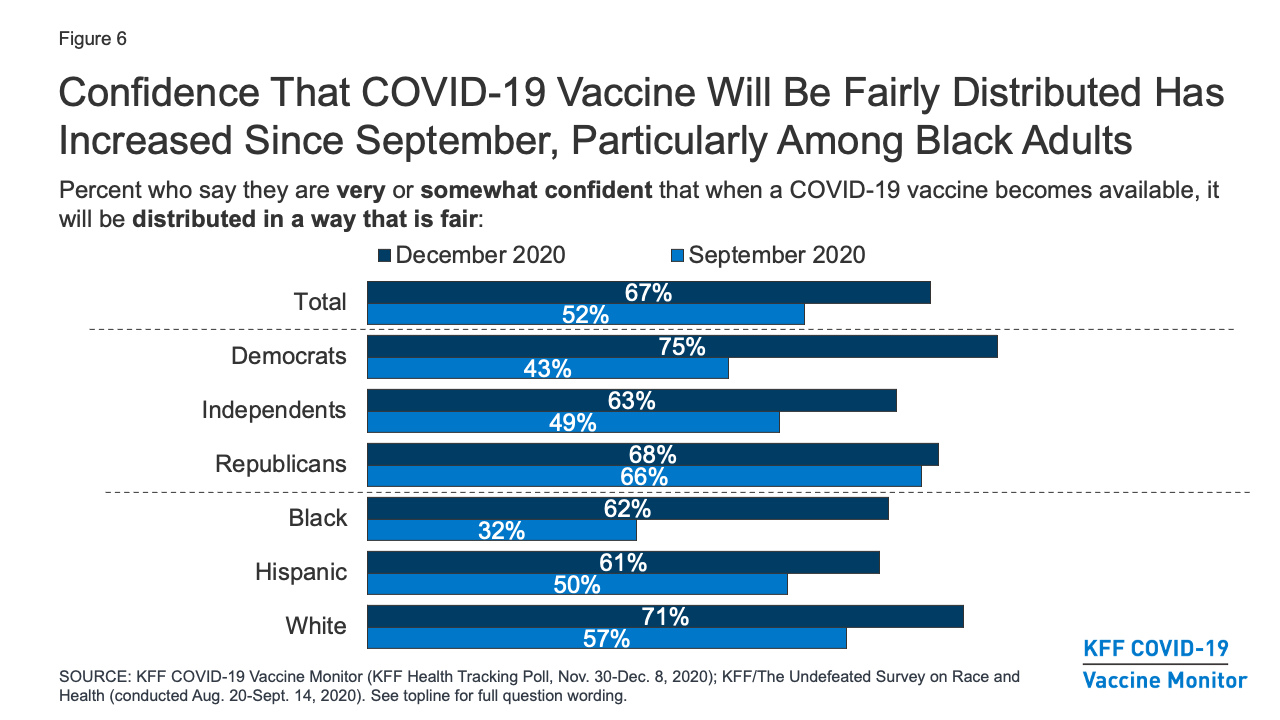
Kff Covid 19 Vaccine Monitor December 2020 Kff

Iha Howell Primary Care Primary Care Family Medicine Internal Medicine Pediatrics Care Management In Howell

Covid 19 Testing In Puerto Vallarta Vallarta Adventures
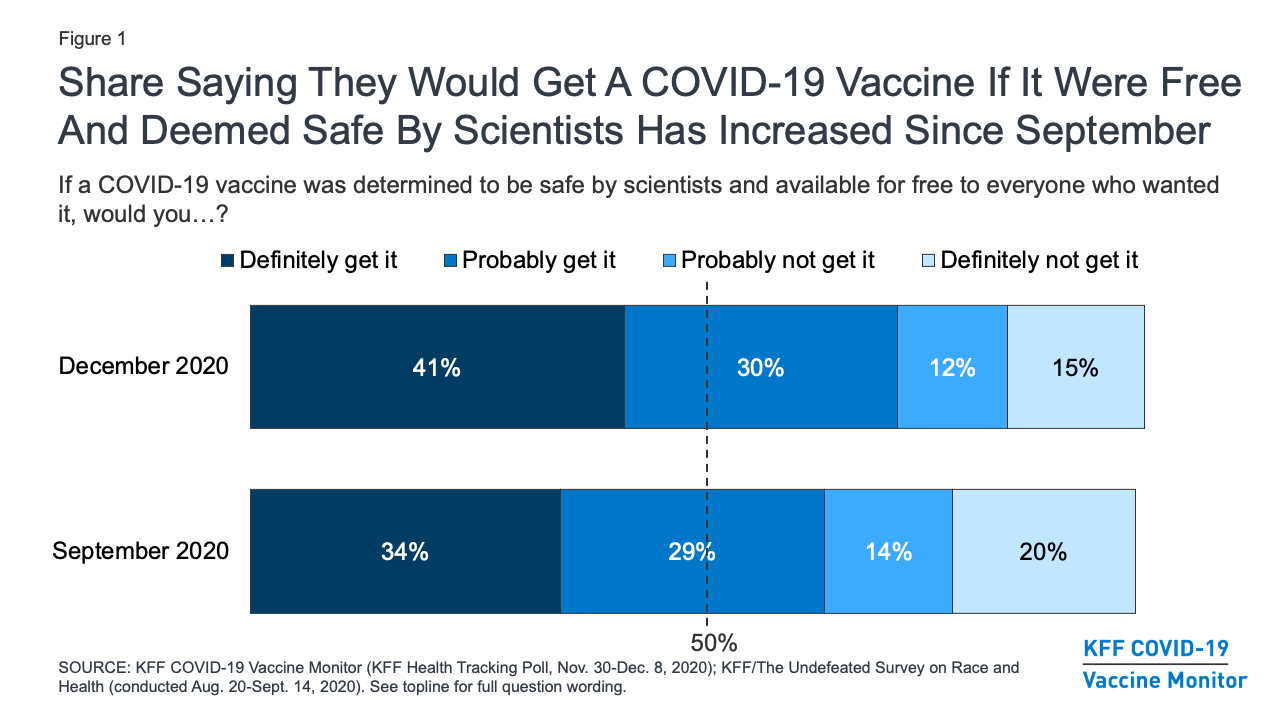
Kff Covid 19 Vaccine Monitor December 2020 Kff

Tests For Covid 19 Are Expensive But They Don T Have To Be

Where Can I Travel In Europe Right Now A Complete List Of Covid 19 Restrictions Euronews

Sars Cov 2 Diagnostic Pipeline Find
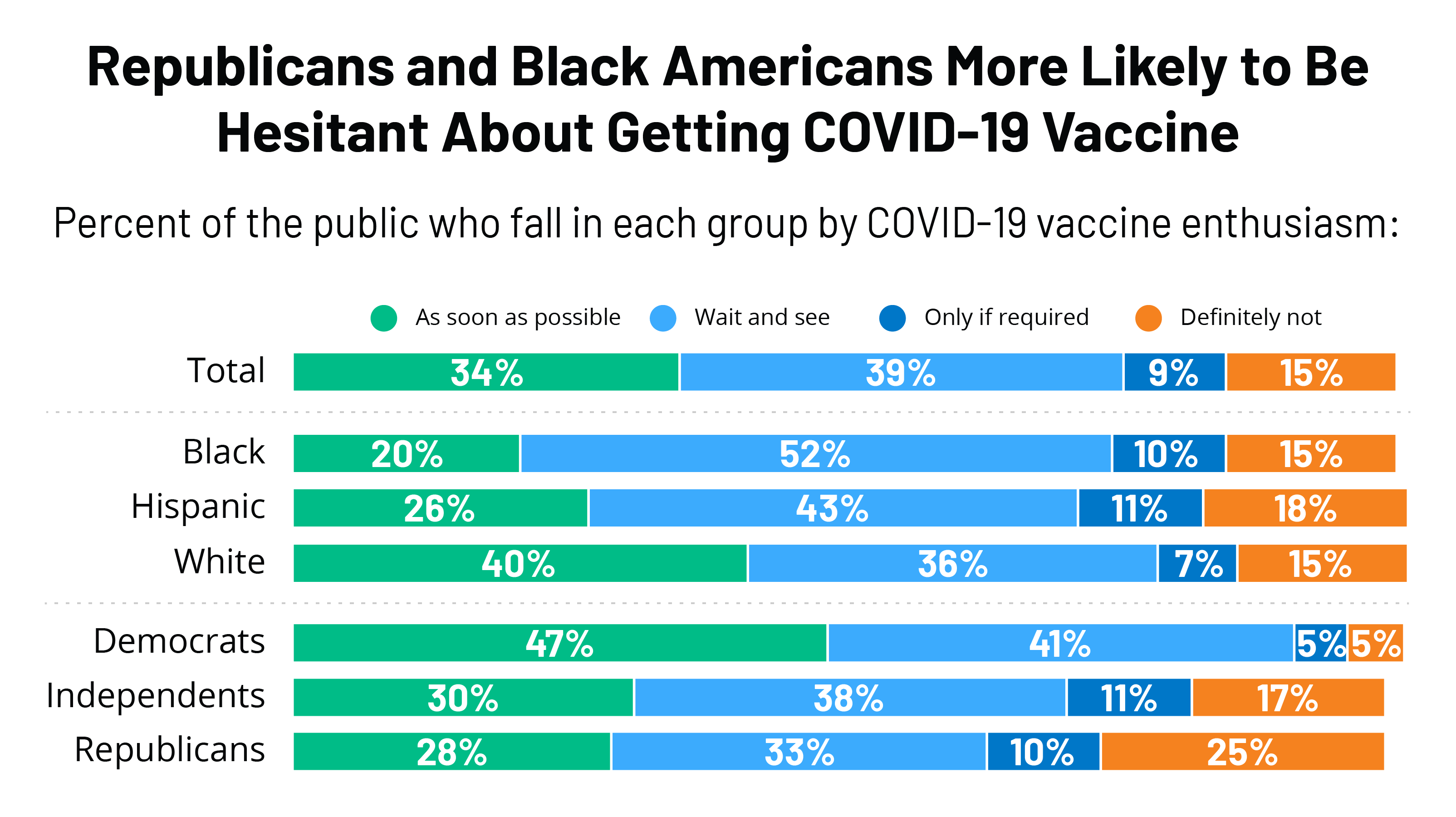
Kff Covid 19 Vaccine Monitor December 2020 Kff

Your Safety Drives Us Uber Blog

Covid 19 Testing In Puerto Vallarta Vallarta Adventures




Posting Komentar untuk "Does Blue Cross Complete Cover Covid Testing"