Does Blue Cross Blue Shield Cover Covid 19 Testing
Were continually making efforts to provide you with the support and guidance you need. COVID-19 pandemic providers should submit ICD-10 code Z20822 for the pre-procedure COVID-19 testing.

Coverage And Costs Highmark Answers
Your Blue Cross and Blue Shield of Illinois BCBSIL health plan gives you access to the care you need during the COVID-19 pandemic.

Does blue cross blue shield cover covid 19 testing. Anthem Issues Updates Regarding COVID-19 Testing and Care to Support Affiliated Health Plan Members. COVID-19 in Missouri - Blue Cross and Blue Shield. However we do cover the cost of testing if a health care provider orders an FDA-approved test and determines that the test is medically necessary.
The vaccines are our most powerful tool to stop the spread of COVID-19. CareFirst will cover with no cost share to the member including our members enrolled in high deductible health plans the appropriate medically necessary diagnostic testing for COVID-19 where it is not covered as part of the Public Health Service response and ensure patient testing and any subsequently needed care are done in close coordination with federal state and public health authorities. Everyone can get tested.
When planning your next getaway please refer to our guide to safe travel. The COVID-19 test is 0 for all members and through Aug. Additionally Florida Blue does not cover tests in the following situations.
Eligible members can earn 50 on their MyBlue Wellness Card when they submit their vaccination record. Blue Cross Blue Shield of Massachusetts Expedites Access to Testing and Care Related to the Novel Coronavirus COVID-19 BOSTON March 6 2020 PRNewswire -- Blue Cross Blue Shield of Massachusetts Blue Cross has been monitoring and responding to the serious challenges posed by the outbreak of coronavirus strain COVID-19 and we are taking immediate steps to expedite access to testing. Lab tests to diagnose COVID-19 are covered at no cost.
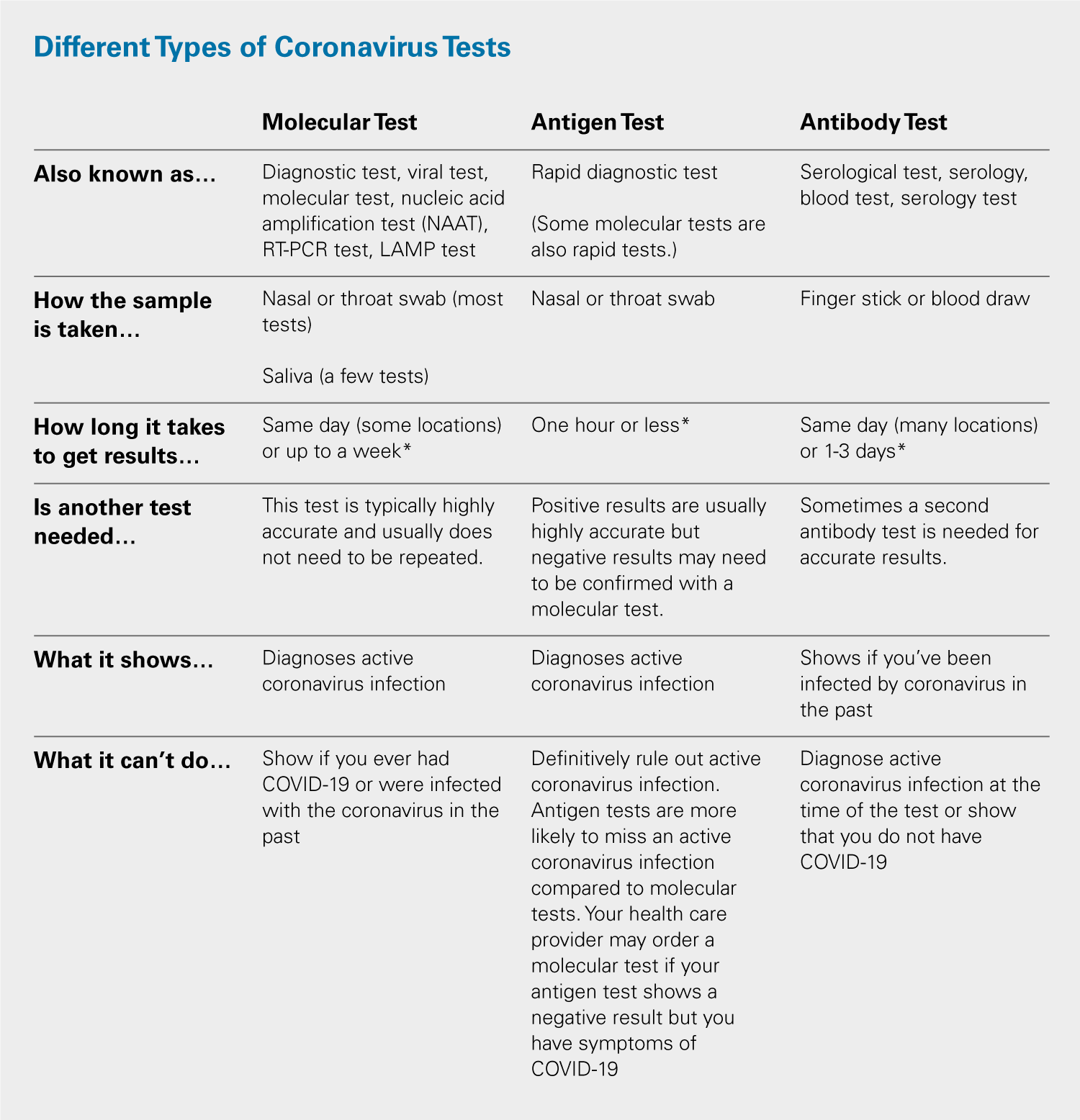
Blue Shield will not cover antibody tests unless ordered by a healthcare provider licensed to order COVID-19 tests and for a rare case in which it is needed to help make a diagnosis. Some may end sooner depending on your plan. Effective immediately BCBSTX will not require preauthorization and will not apply members copays or deductibles for testing to diagnose COVID-19 when medically necessary.
Will Overseas Members in the United Kingdom. No Blue Cross doesnt cover the cost of workplace or occupational screening tests for COVID-19. COVID-19 Test Site Finder.
Virtually using telehealth In a doctors office At an urgent care center or. Check your state guidelines and call the coronavirus testing site before you go to learn about testing criteria availability and hours. COVID-19 screenings or evaluations done.
This includes screenings andor tests that take place at in-person office visits drive-through sites virtual on-line visits and telephone calls. When ordered by your doctor testing diagnosis and treatment for COVID-19 are available to Horizon Blue Cross Blue Shield of New Jersey Horizon BCBSNJ members with zero out-of-pocket costs. Most changes will end with the end of the public health emergency.
Help speed access to COVID-19 testing and treatment and encourage the use of telehealth instead of in person visits to stop the spread of COVID-19. Who can get tested for COVID-19. During the federal public health emergency Blue Shield will continue to waive out-of-pocket costs for copays coinsurance and deductibles for.
Coronavirus test criteria and availability are changing daily. Therefore Blue Cross plans will cover outpatient COVID-19 testing and treatment as well as all telehealth visits without charging members any. Members cost share is waived for COVID-19 testing regardless of testing results.
Blue Cross and Blue Shield of Texas BCBSTX members will have access to coronavirus COVID-19 testing as recommended by the Centers for Disease Control and Prevention CDC and prescribed by health providers. These are covered based on your benefit plan. Anthems affiliated health plans waive member costs for COVID-19 testing while supporting telehealth and 90-day maintenance medication supply.
BCBSTX is waiving your share of the costs for COVID-19 testing and testing-related visits until the end of the Health and Human Services COVID-19 public health emergency order. Doctors visits using telehealth. COVID-19 testing and treatment.
Members will pay no deductible copay or coinsurance for services ranging from doctors visits to hospital stays when their testing or treatment is related to COVID-19. The FDA has approved several vaccines for emergency use authorization. You must be a Blue Cross and Blue Shield Service Benefit Plan member 18 or older with a MyBlue account to earn this reward.
Blue Cross and Blue Shield Companies Announce Coverage of Coronavirus Testing for Members and Other Steps to Expand Access to Coronavirus Care CHICAGO -- Blue Cross Blue Shield Association BCBSA announced today that its network of 36 independent and locally-operated Blue Cross and Blue Shield BCBS companies will waive prior authorizations and increase coverage for COVID-19 as. All Anthem plans will cover medically necessary screening and testing for COVID-19 and will waive all cost shares co-pays coinsurance and deductibles. Employer Testing for COVID-19 o Florida Blue does not cover employer-requested testing under its health plan benefits.
Does my plan cover COVID-19 screening and testing. See below for those not covered This means you do not need to pay out-of-pocket costs copay coinsurance or deductible for tests that are provided or ordered by a healthcare provider. Wherever you may be your health and safety are our priority.
The Blue Cross Blue Shield Service Benefit Plan also known as the Federal Employee Program FEP will cover the administration cost at 100. Blue Shield and Blue Shield Promise cover most diagnostic tests for individuals at no out-of-pocket cost to you. Do your part and get vaccinated by December 31 2021.
Blue Cross will cover the cost of FDA-approved COVID-19 diagnostic and antibody tests that are ordered by an attending healthcare provider who determines testing is medically appropriate. Highmark Blue Cross Blue Shield of Western New York is closely monitoring the COVID-19 Coronavirus situation. 31 were waiving the cost share for covered services for the treatment of those with a positive COVID-19 diagnosis.
These tests should be covered by the employer. When are COVID-19 tests covered. Our COVID-19 website has the most up-to-date.
The health and well-being of our members is our top priority and we remain committed to ensuring our members and customers have access to the care and information they need.

Bcbs Kansas City Claims National Covid 19 Testing Lab Is Disaster Profiteering Modern Healthcare

We Re Continuing To Waive Covid 19 Testing And Treatment Costs For Our Members

Your Frequently Asked Questions About Covid 19 Coronavirus

Coronavirus Covid 19 Resource Center Empire Bluecross Blueshield

Do You Need A Covid Test Wellmark Blue
Developing A Sound Strategy For Testing Screening Your Employees For Covid 19 Blue Cross Blue Shield

Where To Go For Covid 19 Testing And Vaccines Blue Cross And Blue Shield Of Texas

How Blue Cross And Blue Shield Of Nebraska Is Responding To The Covid 19 Pandemic And What You Need To Know Newsroom Blue Cross And Blue Shield Of Nebraska

Covid 19 Testing And Treatment Blue Cross Blue Shield Of Vermont
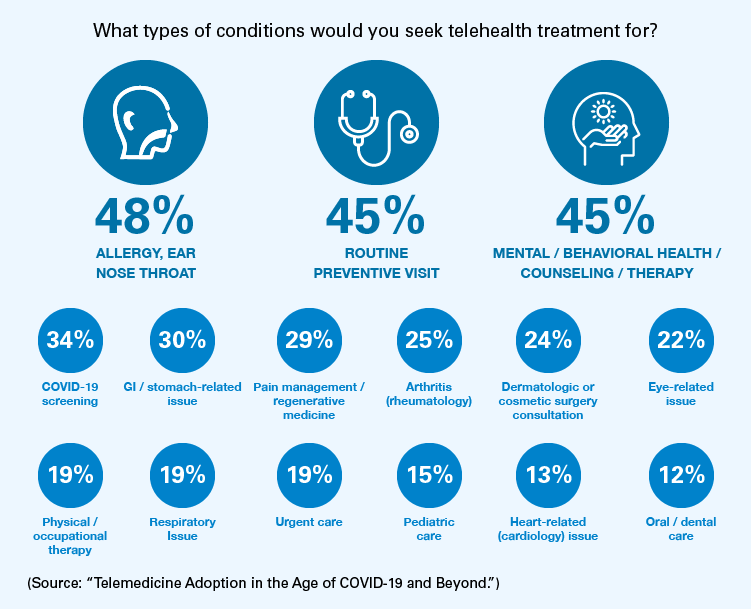
Increasing Telehealth And Virtual Care In The Covid 19 Era Blue Cross Blue Shield

Blue Cross Nc To Cover Member Cost Of Coronavirus Test Blue Cross Nc

Your Guide To No Cost Testing And Treatment As Covid 19 Surges
Azblue Coronavirus For Providers
For Your Employees Covid 19 Resources Bcbsm

Testing For Covid 19 Faqs Blue Shield Of Ca

Blue Cross Coverage Of Covid 19 Testing What To Know Mibluesperspectives

Covid 19 Provider Resources Blue Cross Nc



Posting Komentar untuk "Does Blue Cross Blue Shield Cover Covid 19 Testing"